Blog 2| HEaL Institute & IJME – Covid-19 Insights | April 4, 2020
WHO’s ‘Guidance for Managing Ethical Issues for Infectious Disease Outbreaks’: Key Features and Genesis | Sunita V S Bandewar

The World Health Organisation (WHO) developed a document entitled ‘Guidance for Managing Ethical Issues for Infectious Disease Outbreaks’ (henceforth ‘Guidance’) in response to the Ebola Virus Disease (EVD) outbreak in West Africa (2014-2016). The global community was confronted with wide ranging ethical issues both in clinical research, and health care delivery domains due to EVD pandemic. These concerns arose in other outbreaks, too but during those periods the focus had generally been on a specific pathogen, such as, Severe Acute Respiratory Syndrome (SARS), pandemic influenza, Multi Drug Resistant Tuberculosis (MDR TB), and Middle East Respiratory syndrome (MERS). The stated purpose of this Guidance is “…to look beyond issues specific to a particular epidemic pathogen and instead focus on the cross-cutting ethical issues that apply to infectious disease outbreaks generally.” This document notes that during such public health emergencies, decisions are often made on an urgent basis, in a climate of fear, distrust, and scientific uncertainty, and social and institutional disruption.
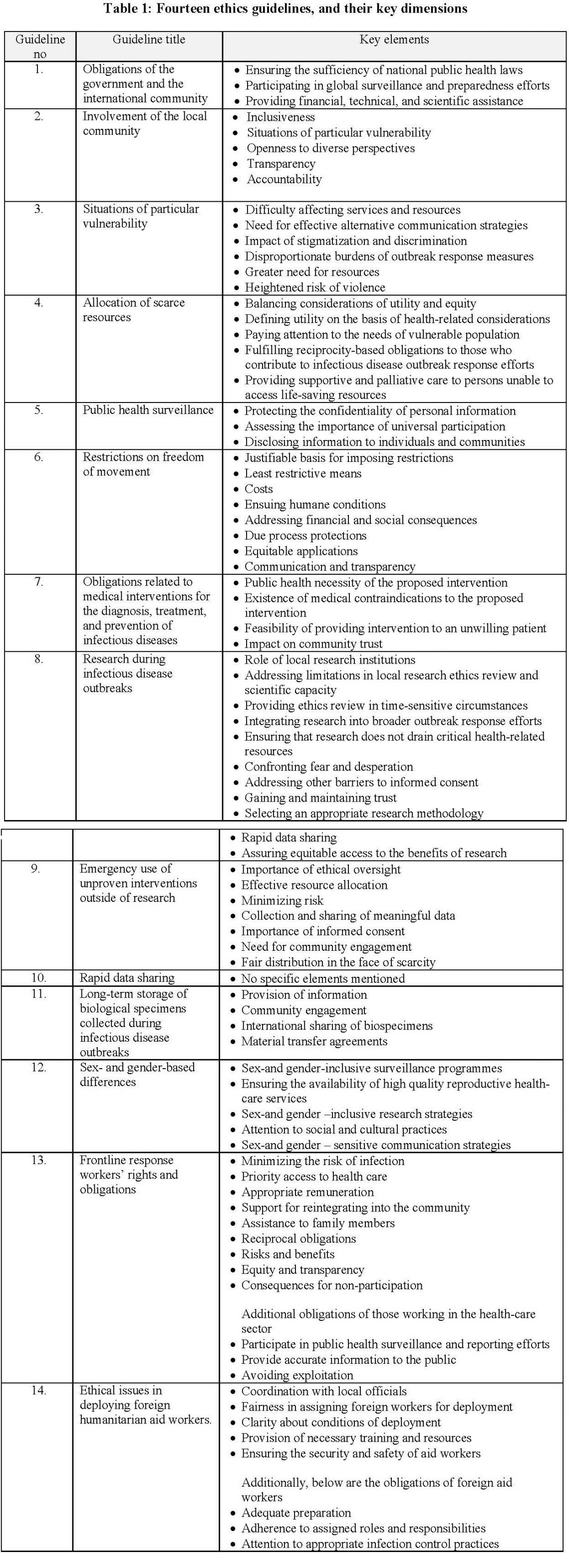
This Guidance document enlists seven core ethics principles and 14 ethics guidelines (Table 1) comprising a broader ethics framework to be complied with by various constituencies including governments during global public health emergencies, such as the on-going Covid-19 pandemic. The seven core ethics principles are: 1. justice, 2. beneficence, 3. utility, 4. respect for persons, 5. liberty, 6. solidarity, and 7. reciprocity. The 14 ethical principles are: 1. Obligations of the government and the international community; 2. Involvement of the local community, 3. Situations of particular vulnerability, 4. Allocation of scarce resources, 5. Public health surveillance, 6. Restrictions on freedom of movement, 7. Obligations related to medical interventions for the diagnosis, treatment, and prevention of infectious diseases, 8. Obligations related to medical interventions for the diagnosis, treatment, and prevention of infectious diseases, 9. Emergency use of unproven interventions outside of research, 10. Rapid data sharing, 11. Long-term storage of biological specimens collected during infectious disease outbreaks, 12. Sex- and gender-based differences, 13. Frontline response workers’ rights and obligations, 14. Ethical issues in deploying foreign humanitarian aid workers.
The document is organised around fourteen specific guidelines, each of which addresses key aspects of epidemic planning and response (Table 1). Each of these guidelines are introduced by a series of questions that illustrate the scope of the ethical issues. These are then followed by a more detailed discussion that articulates the rights and obligations of relevant stakeholders drawing upon the aforesaid relevant core ethics principles. It is also accompanied by a training manual with case studies. The manual is titled, ‘Ethics in epidemics, emergencies and disasters – Training Manual’.
Genesis, processes, deliberations and prioritie
I briefly present the genesis of the Guidance and processes that were put in place. This is meant to help us appreciate the legitimacy it lends to the Guidance until further revisions take place to respond to newer challenges by newer pandemics.
Against the backdrop of EVD outbreak of 2014 in Western Africa, the WHO invited and hosted consultations involving experts from around the world during the period between Aug 2014 and Nov 2015. It was to discuss the Ebola outbreak focusing on ethical issues involved both in research and interventions related matters.
In today’s globalised world the processes involved for developing globally applicable guidance by United Nations agencies such as the World Health Organisation (WHO) tend to serve as proxy indicators of ethics of developing them (procedural justice). It also demonstrates the commitment of the global community and entities such as WHO to respond to public health emergencies threatening health security of local communities and potentially global communities subsequently (solidarity). Other important elements of ethics of developing such guidance, broadly speaking, would be ensuring representation from around the world, especially from the countries affected with the outbreak (equity) in the international consultative processes; and making deliberations of these consultations public and accessible to the global community (transparency). If not initially, in the later part of consultations efforts were made to hear from additional experts and stakeholders, including survivors of the recent Ebola outbreak. During those times, though, WHO was critiqued for delayed response. As well, in my assessment, there should have been more representation from the EVD affected countries in West Africa and other resource limited countries.
The Guidance is not without gaps and critique and yet in the current pandemic of Covid-19, these are the most relevant and comprehensive ones which should guide our response at all levels and in all domains to the ongoing Covid-19 pandemic. We need to ensure compliance with reasonable global ethics standards.
In the closing, I would like to mention that this Guidance will also help the government and state administrators who have to take difficult decisions regarding balancing rights of individuals and public good, and confronting situation of priority setting given the scare resources available to respond to the pandemic. It will also help avert excesses that would be triggered by invocation of the arcane Epidemic Diseases Act 1897. We have already witnessed such excesses over the past few weeks.